

Revised: September 2000
ADENOSCANŽ
(adenosine injection)
FOR INTRAVENOUS INFUSION ONLY
DESCRIPTION
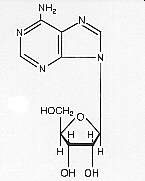
Adenosine is an endogenous
nucleoside occurring in all cells of the body. It is chemically
6-amino-9-beta-D-ribofuranosyl-9-H-purine and has the following structural
formula:
|
C10H13N5O4
267.24 |
Adenosine is a white crystalline powder. It is soluble in water and practically insoluble in alcohol. Solubility increases by warming and lowering the pH of the solution.
Each Adenoscan vial contains a sterile, non-pyrogenic solution of adenosine 3 mg/mL and sodium chloride 9 mg/mL in Water for Injection, q.s. The pH of the solution is between 4.5 and 7.5.
Mechanism of Action
Adenosine is a potent vasodilator in
most vascular beds, except in renal afferent arterioles and hepatic veins where
it produces vasoconstriction. Adenosine is thought to exert its pharmacological
effects through activation of purine receptors (cell-surface A1 and
A2 adenosine receptors). Although the exact mechanism by which
adenosine receptor activation relaxes vascular smooth muscle is not known, there
is evidence to support both inhibition of the slow inward calcium current
reducing calcium uptake, and activation of adenylate cyclase through
A2 receptors in smooth muscle cells. Adenosine may also lessen
vascular tone by modulating sympathetic neurotransmission. The intracellular
uptake of adenosine is mediated by a specific transmembrane nucleoside transport
system. Once inside the cell, adenosine is rapidly phosphorylated by adenosine
kinase to adenosine monophosphate, or deaminated by adenosine deaminase to
inosine. These intracellular metabolites of adenosine are not vasoactive.
Myocardial uptake of thallium-201 is directly proportional to coronary blood flow. Since Adenoscan significantly increases blood flow in normal coronary arteries with little or no increase in stenotic arteries, Adenoscan causes relatively less thallium-201 uptake in vascular territories supplied by stenotic coronary arteries i.e., a greater difference is seen after Adenoscan between areas served by normal and areas served by stenotic vessels than is seen prior to Adenoscan.
Hemodynamics
Adenosine produces a direct negative
chronotropic, dromotropic and inotropic effect on the heart, presumably due to
A1-receptor agonism, and produces peripheral vasodilation, presumably
due to A2-receptor agonism. The net effect of Adenoscan in humans is
typically a mild to moderate reduction in systolic, diastolic and mean arterial
blood pressure associated with a reflex increase in heart rate. Rarely,
significant hypotension and tachycardia have been observed.
Pharmacokinetics
Intravenously administered adenosine is
rapidly cleared from the circulation via cellular uptake, primarily by
erythrocytes and vascular endothelial cells. This process involves a specific
transmembrane nucleoside carrier system that is irreversible, nonconcentrative,
and bidirectionally symmetrical. Intracellular adenosine is rapidly metabolized
either via phosphorylation to adenosine monophosphate by adenosine kinase, or
via deamination to inosine by adenosine deaminase in the cytosol. Since
adenosine kinase has a lower Km and Vmax than adenosine
deaminase, deamination plays a significant role only when cytosolic adenosine
saturates the phosphorylation pathway. Inosine formed by deamination of
adenosine can leave the cell intact or can be degraded to hypoxanthine,
xanthine, and ultimately uric acid. Adenosine monophosphate formed by
phosphorylation of adenosine is incorporated into the high-energy phosphate
pool. While extracellular adenosine is primarily cleared by cellular uptake with
a half-life of less than 10 seconds in whole blood, excessive amounts may be
deaminated by an ecto-form of adenosine deaminase. As Adenoscan requires no
hepatic or renal function for its activation or inactivation, hepatic and renal
failure would not be expected to alter its effectiveness or tolerability.
Clinical Trials
In two crossover comparative studies
involving 319 subjects who could exercise (including 106 healthy volunteers and
213 patients with known or suspected coronary disease), Adenoscan and exercise
thallium images were compared by blinded observers. The images were concordant
for the presence of perfusion defects in 85.5% of cases by global analysis
(patient by patient) and up to 93% of cases based on vascular territories. In
these two studies, 193 patients also had recent coronary arteriography for
comparison (healthy volunteers were not catheterized). The sensitivity (true
positive Adenoscan divided by the number of patients with positive (abnormal)
angiography) for detecting angiographically significant disease (>50%
reduction in the luminal diameter of at least one more vessel) was 64% for
Adenoscan and 64% for exercise testing, while the specificity (true negative
divided by the number of patients with negative angiograms) was 54% for
Adenoscan and 65% for exercise testing. The 95% confidence limits for Adenoscan
sensitivity were 56% to 78% and for specificity were 37% to 71%.
Intracoronary doppler flow catheter studies have demonstrated that a dose of intravenous Adenoscan of 140 mcg/kg/min produces maximum coronary hyperemia (relative to intracoronary papaverine) in approximately 95% of cases within two to three minutes of the onset of infusion. Coronary blood flow velocity returns to basal levels within one to two minutes of discontinuing the Adenoscan infusion.
Intravenous Adenoscan is indicated as an adjunct to thallium-201 myocardial perfusion scintigraphy in patients unable to exercise adequately (see WARNINGS).
Intravenous Adenoscan (adenosine injection) should not be administered to individuals with:
Fatal Cardiac Arrest, Life Threatening Ventricular Arrhythmias, and
Myocardial Infarction.
Fatal cardiac arrest, sustained ventricular
tachycardia (requiring resuscitation), and nonfatal myocardial infarction have
been reported coincident with Adenoscan infusion. Patients with unstable angina
may be at greater risk. Appropriate resuscitative measures should be
available.
Sinoatrial and Atrioventricular Nodal Block
Adenoscan
(adenosine injection) exerts a direct depressant effect on the SA and AV nodes
and has the potential to cause first-, second- or third-degree AV block, or
sinus bradycardia. Approximately 6.3% of patients develop AV block with
Adenoscan, including first-degree (2.9%), second-degree (2.6%), and third-degree
(0.8%) heart block. All episodes of AV block have been asymptomatic, transient,
and did not require intervention. Adenoscan can cause sinus bradycardia.
Adenoscan should be used with caution in patients with pre-existing first-degree
AV block or bundle branch block and should be avoided in patients with
high-grade AV block or sinus node dysfunction (except in patients with a
functioning artificial pacemaker). Adenoscan should be discontinued in any
patient who develops persistent or symptomatic high-grade AV block. Sinus pause
has been rarely observed with adenosine infusions.
Hypotension
Adenoscan (adenosine injection) is a potent
peripheral vasodilator and can cause significant hypotension. Patients with an
intact baroreceptor reflex mechanism are able to maintain blood pressure and
tissue perfusion in response to Adenoscan by increasing heart rate and cardiac
output. However, Adenoscan should be used with caution in patients with
autonomic dysfunction, stenotic valvular heart disease, pericarditis or
pericardial effusions, stenotic carotid artery disease with cerebrovascular
insufficiency, or uncorrected hypovolemia, due to the risk of hypotensive
complications in these patients. Adenoscan should be discontinued in any patient
who develops persistent or symptomatic hypotension.
Hypertension
Increases in systolic and diastolic pressure
have been observed (as great as 140 mm Hg systolic in one case) concomitant with
Adenoscan infusion; most increases resolved spontaneously within several
minutes, but in some cases, hypertension lasted for several hours.
Bronchoconstriction
Adenoscan (adenosine
injection) is a respiratory stimulant (probably through activation of carotid
body chemoreceptors) and intravenous administration in man has been shown to
increase minute ventilation (Ve) and reduce arterial PCO2 causing
respiratory alkalosis. Approximately 28% of patients experience breathlessness
(dyspnea) or an urge to breathe deeply with Adenoscan. These respiratory
complaints are transient and only rarely require intervention.
Adenosine administered by inhalation has been reported to cause bronchoconstriction in asthmatic patients, presumably due to mast cell degranulation and histamine release. These effects have not been observed in normal subjects. Adenoscan has been administered to a limited number of patients with asthma and mild to moderate exacerbation of their symptoms has been reported. Respiratory compromise has occurred during adenosine infusion in patients with obstructive pulmonary disease. Adenoscan should be used with caution in patients with obstructive lung disease not associated with bronchoconstriction (e.g., emphysema, bronchitis, etc.) and should be avoided in patients with bronchoconstriction and bronchospasm (e.g. asthma). Adenoscan should be discontinued in any patient who develops severe respiratory difficulties.
Drug Interactions
Intravenous Adenoscan (adenosine
injection) has been given with other cardioactive drugs (such as beta adrenergic
blocking agents, cardiac glycosides, and calcium channel blockers) without
apparent adverse interactions, but its effectiveness with these agents has not
been systematically evaluated. Because of the potential for additive or
synergistic depressant effects on the SA and AV nodes, however, Adenoscan should
be used with caution in the presence of these agents.
The vasoactive effects of Adenoscan are inhibited by adenosine receptor antagonists, such as methylxanthines (e.g., caffeine and theophylline). The safety and efficacy of Adenoscan in the presence of these agents has not been systematically evaluated.
The vasoactive effects of Adenoscan are potentiated by nucleoside transport inhibitors, such as dipyridamole. The safety and efficacy of Adenoscan in the presence of dipyridamole has not been systematically evaluated.
Whenever possible, drugs that might inhibit or augment the effects of adenosine should be withheld for at least five half-lives prior to the use of Adenoscan.
Carcinogenesis, Mutagenesis, Impairment of Fertility
Studies
in animals have not been performed to evaluate the carcinogenic potential of
Adenoscan (adenosine injection). Adenosine was negative for genotoxic potential
in the Salmonella (Ames Test) and Mammalian Microsome Assay.
Adenosine, however, like other nucleosides at millimolar concentrations present for several doubling times of cells in culture, is known to produce a variety of chromosomal alterations.
Fertility studies in animals have not been conducted with adenosine.
Pregnancy Category C
Animal reproduction studies have not
been conducted with adenosine; nor have studies been performed in pregnant
women. Because it is not known whether Adenoscan can cause fetal harm when
administered to pregnant women, Adenoscan should be used during pregnancy only
if clearly needed.
Pediatric Use
The safety and effectiveness of Adenoscan in
patients less than 18 years of age have not been established.
Geriatric Use
Clinical studies of Adenoscan did not include
sufficient numbers of subjects aged younger than 65 years to determine whether
they respond differently. Other reported experience has not revealed clinically
relevant differences of the response of elderly in comparison to younger
patients. Greater sensitivity of some older individuals, however, cannot be
ruled out.
The following reactions with an incidence of at least 1% were reported with intravenous Adenoscan among 1421 patients enrolled in controlled and uncontrolled U.S. clinical trials. Despite the short half-life of adenosine, 10.6% of the side effects occurred not with the infusion of Adenoscan but several hours after the infusion terminated. Also, 8.4% of the side effects that began coincident with the infusion persisted for up to 24 hours after the infusion was complete. In many cases, it is not possible to know whether these late adverse events are the result of Adenoscan infusion.
| Flushing |
44% |
| Chest discomfort |
40% |
| Dyspnea or urge to breathe deeply |
28% |
| Headache |
18% |
| Throat, neck or jaw discomfort |
15% |
| Gastrointestinal discomfort |
13% |
| Lightheadedness/dizziness |
12% |
| Upper extremity discomfort |
4% |
| ST segment depression |
3% |
| First-degree AV block |
3% |
| Second-degree AV block |
3% |
| Paresthesia |
2% |
| Hypotension |
2% |
| Nervousness |
2% |
| Arrhythmias |
1% |
Adverse experiences of any severity reported in less than 1% of patients include:
Body as a whole: back discomfort; lower extremity discomfort;
weakness.
Cardiovascular System: nonfatal myocardial infarction;
life-threatening ventricular arrhythmia; third-degree AV block; bradycardia;
palpitation; sinus exit block; sinus pause; sweating; T-wave changes;
hypertension (systolic blood pressure > 200 mm Hg).
Central Nervous
System: drowsiness; emotional instability; tremors.
Genital/Urinary
System: vaginal pressure; urgency.
Respiratory System:
cough.
Special Senses: blurred vision; dry mouth; ear discomfort;
metallic taste; nasal congestion; scotomas; tongue discomfort.
The half-life of adenosine is less than 10 seconds and side effects of Adenoscan (when they occur) usually resolve quickly when the infusion is discontinued, although delayed or persistent effects have been observed. Methylxanthines, such as caffeine and theophylline, are competitive adenosine receptor antagonists and theophylline has been used to effectively terminate persistent side effects. In controlled U.S. clinical trials, theophylline (50-125 mg slow intravenous injection) was needed to abort Adenoscan side effects in less than 2% of patients.
For intravenous infusion only.
Adenoscan should be given as a continuous peripheral intravenous infusion.
The recommended intravenous dose for adults is 140 mcg/kg/min infused for six minutes (total dose of 0.84 mg/kg).
The required dose of thallium-201 should be injected at the midpoint of the Adenoscan infusion (i.e., after the first three minutes of Adenoscan). Thallium-201 is physically compatible with Adenoscan and may be injected directly into the Adenoscan infusion set.
The injection should be as close to the venous access as possible to prevent and inadvertent increase in the dose of Adenoscan (the contents of the IV tubing) being administered.
There are no data on the safety or efficacy of alternative Adenoscan infusion protocols.
The safety and efficacy of Adenoscan administered by the intracoronary route have not been established.
The following Adenoscan infusion nomogram may be used to determine that appropriate infusion rate corrected for total body weight:
|
Patient Weight |
Infusion Rate | |
|
kg |
lbs |
mL/min |
|
45 |
99 |
2.1 |
|
50 |
110 |
2.3 |
|
55 |
121 |
2.6 |
|
60 |
132 |
2.8 |
|
65 |
143 |
3.0 |
|
70 |
154 |
3.3 |
|
75 |
165 |
3.5 |
|
80 |
176 |
3.8 |
|
85 |
187 |
4.0 |
|
90 |
198 |
4.2 |
This nomogram was derived from the following general formula:
Note: Parenteral drug products should be inspected visually for particulate matter and discoloration prior to administration.
Adenoscan (adenosine injection) is supplied as 20 mL and 30 mL vials of
sterile nonpyrogenic solution in normal saline.
| Product Code | NDC No. | |
| 87120 | 0469-0871-20 | 60 mg/20 mL (3 mg/mL) in a 20 mL single-dose, flip-top glass vial, packaged individually and in packages of ten. |
| 87130 | 0469-0871-30 | 90 mg/30 mL (3 mg/mL) in a 30 mL single-dose, flip-top glass vial, packaged individually and in packages of ten. |
Store at controlled room temperature 15°-30°C (59°-86°F)
Do not refrigerate as crystallization may occur. If crystallization has occurred, dissolve crystals by warming at room temperature. The solution must be clear at the time of use.
Contains no preservative. Discard unused portion.
Rx only
Manufactured for:
Fujisawa Healthcare, Inc.
Deerfield, IL 60015
Revised: September 2000